Twenty–Nine Year Summary of Silicosis in Michigan
Posted on bySilicosis is a lung disease caused by exposure to airborne silica. Generally, it causes scarring (pulmonary fibrosis) after 20 or more years of exposure. Since 1988, Michigan has been identifying individuals who develop silicosis with the goal of targeting prevention actions. Michigan’s system is both the longest running and only comprehensive surveillance system for silicosis in the United States. We recently reported on the 1,048 Michigan residents with confirmed silicosis identified over 29 years (Reilly MJ, Timmer SJ, Rosenman KD. The Burden of Silicosis in Michigan, 1988-2016. Annals Am Thoracic Society 2018; 15:1404-1410). Key findings were:
-
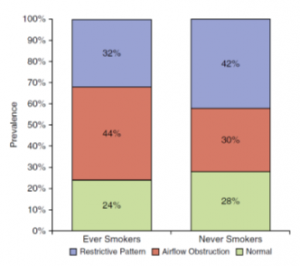
Figure 1*. Restriction, obstruction, and normal spirometry results by cigarette smoking status of confirmed silicosis cases, Michigan, 1988-2016 Classically silicosis was considered a disease that caused stiff, fibrotic lungs and restriction (difficulty fully expanding the lungs). It is now recognized that respirable crystalline silica can also cause chronic obstructive pulmonary disease (COPD). Figure 1 shows that a high percentage of individuals with silicosis have obstructive lung disease (difficulty completely expelling air from the lungs) (30% in never smokers and 44% in ever smokers) and restrictive lung disease (42% in never smokers and 32% in ever smokers). Only 25% of the individuals with silicosis had normal spirometry. This means that silica exposed workers who also smoke cigarettes will have more lung impairment. It also means that doctors, who often are not familiar with the effects of silica, may not recognize when silica contributed to their patients having COPD or emphysema or might miss the diagnosis of silicosis. A particular problem is that when patients smoke, all their respiratory problems might be attributed to smoking, and risk factors like exposure to silica might be missed.
- The incidence of tuberculosis (TB) in individuals with silicosis was 1000-fold greater than in the Michigan general population. Workers with exposure to silica should be tested for TB with either a skin or blood test.
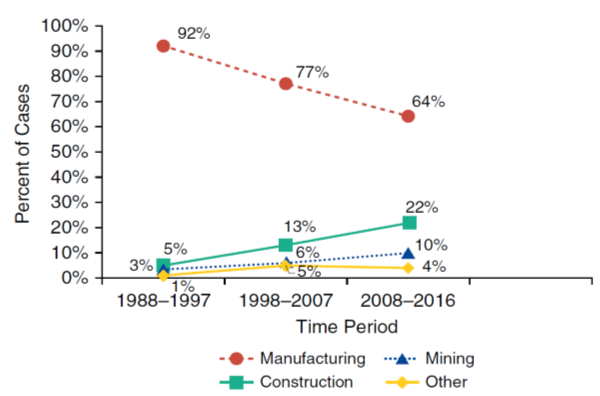
- The source of silica exposure in Michigan causing silicosis has changed over time. The percentage occurring among foundry workers has decreased while the percentage occurring among construction workers has increased (Figure 2). In some states, mining and the manufacture of toilet bowls and sinks will be the major sources of silica exposure. Newer sources of exposures are in the granite and synthetic stone counter top industry, and extraction of natural gas and oil by horizontal drilling and hydraulic fracturing (fracking). The continued use of silica in abrasive blasting operations is an ongoing source of exposure.
- Respiratory diseases are the underlying cause of death on the death certificate in 45% of individuals with silicosis in Michigan (COPD 14%, lung cancer 11%, unspecified interstitial fibrosis or respiratory failure 10%, pneumonia 6%, asbestosis or non-specified pneumoconiosis 3%, tuberculosis 0.5%, and sarcoidosis 0.5%). These percentages illustrate not only the respiratory morbidity of silicosis, but also that the doctors completing cause of death on the death certificate are often not aware of the decedent’s medical history (i.e. only 11% of individuals with the advanced form of silicosis, progressive massive fibrosis, have silicosis listed on the death certificate).
- Medicare is paying for most of the medical costs associated with silicosis in Michigan. The percentage of workers with silicosis applying for workers’ compensation has dropped from 42% in the 1988-1997 decade to 16% in the most recent period.
The new OSHA silica standard, which lowered the allowable amount of silica in the workplace, also requires for the first time that employers provide medical testing including chest x-ray, breathing tests and TB tests for workers exposed to silica. (https://www.osha.gov/dsg/topics/silicacrystalline/health_effects_silica.html).
The standard requires the mandatory referral to a board-certified Pulmonologist or Occupational Medicine physician if the worker has a 1/0 profusion or greater classification on their radiography when read by a “B” reader. A “B” reader is a physician certified by NIOSH to classify films for pneumoconiosis. There are 165 “B” readers in the United States. The medical component of the standard is in effect in the construction industry and will be a requirement in general industry, including foundries, in 2020.
Michigan has a uniquely intense state-based surveillance program for silicosis. It is important to the rest of the country because it identifies contemporary industries and occupations that are still at risk.
Despite improvement in workplace controls for silica, with the new OSHA requirement for medical screening, we expect to see an increase in the number of individuals with silicosis. Employers and employees need to be aware of the hazards of silica, which in addition to silicosis are lung cancer, COPD, TB, chronic kidney failure, rheumatoid arthritis and scleroderma. Substitution of alternative abrasive material, engineering controls and personal protective equipment all play a role in reducing the risk. Workers with exposure to silica, who are being evaluated by their primary care doctors, need to educate their doctors of the diseases associated with silica and the importance of having a “B” reader review their chest x- ray.
Funding for Michigan’s silicosis surveillance comes from NIOSH. More information about this funding can be found at: https://www.cdc.gov/niosh/topics/surveillance/ords/statebasedsurveillance.html and https://www.cdc.gov/niosh/topics/surveillance/ords/statesurveillance/silicosis.html.
We are interested in your thoughts and comments on this summary.
Kenneth D. Rosenman, MD, is a Professor of Medicine and Chief of the Division of Occupational and Environmental Medicine at Michigan State University.
Mary Jo Reilly, MS, epidemiologist, Division of Occupational and Environmental Medicine at Michigan State University.
*Figures 1and 2 are reprinted with permission of the American Thoracic Society. Copyright © 2019 American Thoracic Society. Annals of the American Thoracic Society is an official journal of the American Thoracic Society.
Posted on by

