Infectious Diseases: Precision Medicine for Public Health
Posted on by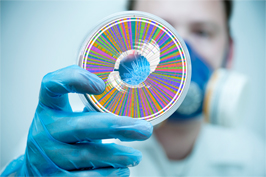 Until now, most medical treatments have been designed for the “average patient.” As a result of this “one-size-fits-all” approach, treatments can be very successful for some patients but not for others. Precision Medicine, on the other hand, is an innovative approach that takes into account individual differences in people’s genes, environments, and lifestyles.
Until now, most medical treatments have been designed for the “average patient.” As a result of this “one-size-fits-all” approach, treatments can be very successful for some patients but not for others. Precision Medicine, on the other hand, is an innovative approach that takes into account individual differences in people’s genes, environments, and lifestyles.
The Precision Medicine Initiative
NIH’s research strategy for precision medicine, outlined recently in the New England Journal of Medicine, appeals broadly to biomedical researchers and others with an interest in individualized health care. Some public health advocates, however, see huge new investments in biological research as an opportunity cost, drawing attention and resources away from research on social determinants of health and population-level interventions. Will precision medicine pay off for a few people at the expense of the population?
The most commonly cited examples of precision medicine—rare disease diagnostics and targeted anti-cancer drugs—clearly pertain to medical specialties like clinical genetics and molecular oncology. Often overlooked, however, is the most fully realized application of precision medicine so far: in infectious diseases, where advances in genomics are already changing both medical and public health practice.
Increasingly automated, standardized and affordable molecular technologies are being integrated into the diagnosis, treatment and control of infections. Genome sequencing and molecular tests can enhance both patient care and public health by delivering more timely and precise identification of pathogens, as well as insights into their sources, spread and susceptibility to antibiotics [Box]. CDC’s Advanced Molecular Detection (AMD) initiative is combining these technologies with bioinformatics and epidemiology to enhance public health surveillance, investigations and control of infectious diseases.
| Application | Patient care | Public health |
|---|---|---|
| Pathogen identification | Rapid diagnosis | Outbreak detection |
| Antibiotic selection | Proper treatment | Effective antibiotic use guidelines |
| Vaccines | Better protection | Reduced burden of disease |
Whether treating an infection or investigating an outbreak, identifying the responsible pathogen is fundamental. Diagnostic tests based on detecting pathogen DNA or RNA have evolved over the last 20 years and are now undergoing rapid development. The FDA has cleared or approved 160 microbial nucleic acid-based tests (compared with 58 based on human genetics) and many more are available as laboratory-developed tests. Last year, FDA issued guidance for developers of multiplex tests, which are designed to test for multiple pathogens at once—for example, to distinguish among influenza and other respiratory viruses.
The traditional diagnostic paradigm is to send off diagnostic test after diagnostic test – and still have no solid diagnosis, and treat patients empirically based on our best guess. That’s why we have developed a test to detect a full spectrum of pathogens in a universal test.
Dr. Charles Chiu, UCSF’s one-size-fits-all precision medicine test for infection
When it comes to using research discoveries to improve health, no one slogan fits all. The speed, precision and economies of scale that new technologies can offer are relevant to healthcare and public health alike. The information they generate, however, will produce both new applications and new challenges—such as distinguishing colonization from infection and understanding the full spectrum of mixed infections.
In 2013, the Infectious Diseases Society of America (IDSA), a professional group representing physicians, scientists, and other specialists in infectious diseases, reported on the current diagnostic landscape and made recommendations for further development. Fulfilling the promise of new technologies, said the report, “will require the engagement and coordination of a number of stakeholders, including Congress, funding and regulatory bodies, public health agencies, the diagnostics industry, healthcare systems, professional societies, and individual clinicians.”
Posted on by


